Addison’s Disease is an endocrine (hormonal) disease of the adrenal glands of dogs (it’s very rare in cats) involves inadequate hormone levels of cortisol (cortisone) and electrolytes (sodium and potassium). The scientific name for this disease is hypoadrenocorticism. This unusual disease can show a vast array of different symptoms, symptoms that can mimic other diseases.
The University of California at Davis vet school has been using Artificial Intelligence (AI) to aid in diagnosis.
The Canine Genetic Analysis Project at UC Davis is using genetics to help in diagnosis also.
There is even a version of this disease called “atypical”, which adds to the complexity. Because there can be such a variety of symptoms, Addison’s disease is sometimes known as the great pretender or great imitator. In any dog that is ill our veterinarians keep this disease in mind.
Addison’s disease is the opposite of another problem with the adrenal glands called Cushing’s Disease (hyperadrenocorticism). In Addison’s there is not enough cortisol, in Cushing’s, there is too much cortisol.
Some dogs with Addison’s can collapse. This is a medical emergency requiring immediate veterinary care. The Long Beach Animal Hospital, staffed with emergency vets, is available until the evenings 7 days per week to help if your dog or cat is having any problem, especially if it is collapsed, breathing hard, or bleeding.
Think of us as your Long Beach Animal Emergency Center to help when you need us for everything from minor problems to a major emergency. We serve all of Los Angeles and Orange county with our Animal Emergency Center Long Beach, and are easily accessible to most everyone in southern California via Pacific Coast Hwy or the 405 freeway.
If you have an emergency that can be taken care of by us at the Animal Emergency Hospital Long Beach always call us first (562-434-9966) before coming. This way our veterinarians can advise you on what to do at home and so that our staff and doctor can prepare for your arrival. To learn more please read our Emergency Services page.
We have an interesting page on adrenal disease in ferrets, which causes different symptoms in the ferret compared to dogs and cats.
Addison’s is named after a physician in 1849’s who discovered this disease. President John Kennedy suffered from the human version of this disease. You can learn more about Addison’s Disease and how at affects people from the Mayo Clinic.
Edward Feldman, a veterinarian at the UC Davis veterinary school is an endocrinologist that has been instrumental in understanding this disease.
The Merck Veterinary Manual as some information on this disease also.
This is Buddy with his happy mom. He has Addison’s, and has responded well to treatment and is back to normal for over the last 7 years.
Addison’s Disease Nomenclature
Several medical terms and abbreviations relate directly to Addison’s that will be used on this page:
| glucocorticoids – Cortisol | tachypnea-increased respiratory rate |
| exogenous cortisone– supplemental cortisone by mouth or injection | bradycardia– abnormally slow heart rate |
| catabolic steroid– cortisol and its equivalent | polyuria– excess urinating |
| anabolic steroid– opposite of catabolic, testosterone is the most common one | polydipsia– excess drinking |
| hyperkalemia- high potassium (K) level in the bloodstream | PU/PD– polyuria and polydipsia |
| tachycardia -abnormally fast heart rate | mineralocorticoid-hormone that affects sodium and potassium |
| hypoglycemia– low blood glucose (sugar) level | iatrogenic– caused by something a person does as opposed to happening naturally. |
| hyponatremia- low sodium (Na) in the bloodstream | ACTH– adrenocorticotrophic hormone |
| atrophy-an organ that is smaller than it should be | adrenomegaly– enlarged adrenal gland |
| anemia– low red blood cells | microcardia- small heart |
| cortisol– Cortisone made by the adrenal glands | azotemia– elevated BUN and creatinine |
Adrenal Gland Anatomy
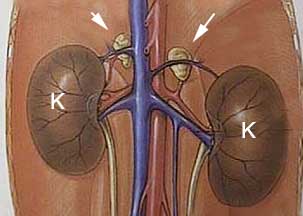
The adrenal glands are paired organs that lay right in front of the kidneys on each side. They are quite small, and measure only a few millimeters in length. This small size is not an indication of their importance though. Even though they are small, the cortisol (cortisone) they secrete, along with their other functions, have great significance to normal physiology.
The arrows point to the paired adrenal glands in front of each kidney. The extensive blood supply to the kidneys and adrenal glands is apparent. In the diagram they are easy to see. They are not so easy to see during ultrasound or exploratory surgery because normally they are small and buried in fat. They do not show up on an X-ray unless they are calcified or much larger than normal.
This is a picture of an enlarged adrenal gland (arrow) that is buried in fat near the kidney (K). It is from a ferret that has an adrenal gland tumor, so the adrenal gland is inflamed and easily visualized. This is not necessarily the case in dogs and cats that have adrenal gland tumors.
The internal architecture of the adrenal gland is made up of several distinct zones:
Cortex
The cortex (outer shell) of the adrenal gland is made up of 3 anatomical parts:
Zona Glomerulosa
This is the outer layer of the adrenal gland. This section secretes the mineralcorticoid aldosterone. Aldosterone is vital to proper sodium and potassium regulation. Aldosterone has a role in maintaining blood pressure.
Zona Fasciculata
This is the next layer as you go inward, and produces the glucocorticoid cortisol. The cells in this area are the ones that cause Cushing’s when they secrete cortisol in excess.
Zona Reticularis
As we continue inward we come across this section that secretes the sex hormones known as androgens (male sex hormones), estrogen (female sex hormones), and sex steroids. These are usually secreted in such small amounts as to be of no major significance in healthy animals. The gonads in dog and cats secrete most of the sex hormones.
Medulla
This consists of the very center of the adrenal gland. It secretes hormones called catecholamines. The two important ones are epinephrine (adrenaline) and norepinephrine.
Physiology
The tiny adrenal glands have a profound influence on many internal organs. The hormones they secrete work in unison with other hormones and internal organs, particularly the liver, and have an enormous effect on physiology.
These hormones interact with many other hormones that have the opposite effect, usually in some type of feedback mechanism that is monitored by the brain. This interaction is complex, so only a summary of adrenal hormone physiology is presented.
The adrenal glands secrete several important hormones, most of which are synthesized from cholesterol. We will explain 3 of them; cortisol, aldosterone, and epinephrine:
Cortisol
Cortisol maintains a normal blood glucose level, facilitates metabolism of fat, and supports the vascular and nervous systems. It affects the skeletal muscles, the red blood cell production system, the immune system, and the kidneys. Obviously, it is a very important hormone, and necessary for life.
It is considered a “catabolic steroid”. This means it takes amino acids from the skeletal muscles and, and with help from the liver, converts them to glycogen, the storage form of glucose. These functions are the exact opposite of “anabolic steroids”, the drugs that weightlifters take to increase muscle mass.
The end result of this is an increase in the level of glucose in the bloodstream. The hormone called insulin has the opposite effect on blood glucose, adding to the complexity of this system. You can learn more about insulin by going to our diabetes mellitus page.
The level of cortisol in the bloodstream continually fluctuates as physiologic needs vary. Surgery, infection, stress, fever, and hypoglycemia (low blood sugar) will cause cortisol to increase. This continual fluctuation adds to the difficulty of diagnosing any disease involving cortisol (Addison’s and Cushing’s), because the amount of cortisol in the bloodstream is so variable. A test taken at one moment in time might have different results if taken later.
To control the level of cortisol the hypothalamus and pituitary gland in the brain secrete chemicals into the bloodstream called releasing factors. In the case of the adrenal glands , the hypothalamus secretes a hormone called corticotropin releasing hormone (CRH). This hormone goes to the pituitary gland and stimulates it to release a hormone called adrenocorticotrophic hormone (ACTH).
It is the amount of ACTH circulating in the blood stream that tells the adrenal glands (specifically, the cells at the zona fasciculata) how much cortisol to secrete. There is a negative feedback loop that allows the hypothalamus and pituitary gland to refine precisely how much cortisol circulates in the bloodstream. The more cortisol secreted by the adrenal glands, the less CRH and ACTH secreted. This allows the body to precisely refine the level of cortisol, and to change the level rapidly due to changing physiologic needs.
This negative feedback mechanism is a highly profound adaptation to evolutionary pressures, and is the basis for our survival as a species. Without this, life as we know it, would not exist for us and many species on this planet.
Numerous organ systems are affected by cortisol:
Mineralocorticoids
Aldosterone is the principal mineralocorticoid secreted by the adrenal glands. This hormone is secreted as a response from the kidneys when fluid volume in the bloodstream is decreasing. It involves other hormones called renin and angiotensin.
The end result is an increase in sodium in the bloodstream, with a corresponding increase in blood volume and blood pressure. This increase in blood volume and pressure is because sodium pulls fluid from the intestinal tract, and the area around each cell called the extracellular fluid, into the bloodstream.
This is how we check the blood pressure in a cat.
This hormone also interacts with and affects potassium levels. To further complicate the picture, ACTH also has an affect here, just like it does with cortisol.
Epinephrine (Adrenaline)
This compound, technically called a neurotransmitter, also has hormone-like properties. It is a very powerful chemical that affects all organ systems. It acts very rapidly, with effects remaining only for a short period of time. It is the primary reason the body has the ability to respond to an emergency. This physiologic mechanism is also known as the “flight or fight” response.
Upon stimulation of the central nervous system (ex.-fear or pain), the adrenal medulla is stimulated to secrete epinephrine into the bloodstream. We are all familiar with what happens next. The pupils dilate, the heart rate and blood pressure increase, and the palms get sweaty.
Internally, the body is increasing the blood glucose level, the breathing passages are opened up, more red blood cells are secreted into the circulation, blood is shunted away from the skin and other internal organs, and blood flow is increased to the brain and skeletal muscles.
All of this has the effect of bringing the brain and skeletal muscles extra glucose and oxygen, and accounts for the extra boost of awareness and energy we all feel at this time. For such a small set of organs it is apparent that the paired adrenal glands have a very important role in normal health.
Pathophysiology
When the disease affects the part of the adrenals that secrete cortisol (the zona fasiculata) a vast array of different symptoms can occur. This is because of the profound effects cortisol has on almost all body systems.When the disease affects the part of the adrenals that secrete aldosterone (the zona glomerulosa), then electrolytes like sodium (Na+) and Potassium (K+) are affected.
Sodium and potassium are crucial, along with other electrolytes, and are checked when we submit a blood panel
The overwhelming majority of the adrenal cortex must be affected before it secretes inadequate amounts of cortisol and aldosterone and before any symptoms are noted.
There are 3 forms of this disease:
Primary Hypoadrenocorticism
This classic form of the disease is due to a lack of both mineralocorticoids and glucocorticoids. The zona fasiculata and the zona glomerulosa are both involved. This means the problem is at the adrenal gland itself.
Causes:
-
- Immune system destruction of the adrenal gland due to autoantibodies is the most common cause
- Medication to treat Cushing’s disease (mitotane or trilostane)
- Infection
- Coagulation disease
- Cancer
- Loss of blood supply to the adrenal gland (an infarction)
Secondary Hypoadrenocorticism
This more unusual form of the disease occurs when the zona fasiculata only is involved. This means the problem is at the pituitary and not at the adrenal gland, therefore only cortisol production is compromised and the electrolytes sodium and potassium are not affected.
Causes:
-
- Abruptly stopping oral or injection cortisone that has been administered for a period of time (exogenous cortisone)
- Congenital defects of the pituitary gland
- Cancer or trauma to the hypothalamus
Atypical
This includes all of the dogs classified as secondary, so only cortisol is involved. In these dogs electrolytes are normal, just like in secondary hypoadrenocorticism. What makes this atypical is that fact that many dogs might change to primary during the course of the disease and the electrolytes will have a problem.
This can make treatment difficult, because a pet that is being treated successfully for secondary might need to be treated for primary at some point. This emphasizes the need for close monitoring with blood panels and exams at least every 6 months.
Diagnosis
Signalment
Usually found in female dogs that are middle aged or less. It is more commonly found in dogs that are not spayed (ovariohysterectomy). Atypical Addison’s tends to occur more in the older dog. Certain breeds get this disease more often than others:
-
- Great Danes
- Standard Poodles
- Bearded collies
- Portugese water dogs
- Rottweilers
- Wheaten Terriers
- West Highland White Terriers (Westies)
History
Symptoms are quite variable, and can come and go over months. As a result, it is easy to miss this disease or get it confused with other diseases that have the same symptoms. Symptoms might be mild, or they might be life threatening, and can be found in many other diseases.
In some cases, a pet has been ill in the past, and treated with fluids with a successful outcome, and now the problem has returned. A blood panel in this situation might show a kidney problem due to dehydration, which is why the fluids helped. If this is a recurring problem, Addison’s should be tested for.
We usually give fluids IV (intravenously) or SQ (subcutaneous) like Alex is doing in the above picture. Click on his mug if you want to get a detailed primer on how fluids are a crucial part of how we treat sick animals.
Typical symptoms might include:
-
- lethargy
- inappetence
- weight loss
- diarrhea or dark stools (melena or hematochezia))
- vomiting
- shaking
- dehydration
- shock
- collapse
- drinking and urinating more than usual (PU/PD)
- abdominal pain
- seizures if severely low blood sugar is present
Physical Exam
Just like the symptoms above, the physical exam of a dog with this disease can be quite variable. Typical exam findings we might encounter include:
-
- depression
- pale gums
- tacky gums
- panting
- hair loss
- weak pulse
- increased heart rate (tachycardia) if shock
- decreased heart rate (bradycardia) if potassium is high
- increased respiratory rate (tachypnea)
- low body temperature
- painful abdomen upon palpation
One of the ways we check for pale gums (#2 in the list above) is to do a CRT- capillary refill time. When we push on the pink gums they blanche to white, then go back to pick. If they return to pick in less than 2 seconds it is normal.
Diagnostic Tests
Radiography
X-rays might be helpful in diagnosis, although they are not the primary way this disease is diagnosed. On a radiograph we might find a small heart and liver due to dehydration and shock.
On rare occasions megaesophagus (a dilated esophagus that does not pass food properly to the stomach) might be present. None of these symptoms are diagnostic of Addison’s by themselves, since numerous other diseases can cause these symptoms.
.
The heart is the white object in the center of this radiograph. Compared to the heart in the radiograph below it is small, which might indicate dehydration due to Addison’s.
This is a normal sized heart in a dog
This radiograph of the chest of a dog on its side has the megaesophagus circled in red
The adrenal glands do not show up on an abdominal radiograph unless they are calcified or extremely enlarged, which would be more indicative of Cushing’s and not Addison’s.
We have a detailed page on Radiology if you would like to learn more.
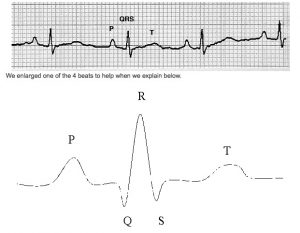
Electrocardiogram (ECG or EKG)
If the potassium is high enough (hyperkalemia) the heart rate might be slow (bradycardia) and there might be changes in the electrocardiogram. There are other causes of hyperkalemia, so this is not diagnostic for Addison’s, it is a clue that Addison’s might be present. The most common cause we see for hyperkalemia is a cat that cannot urinate in the obstructed version of FLUTD (Feline Lower Urinary Tract Disease).
Below is a normal EKG strip for 4 beats of the heart. Below the strip is an enlargement of one beat. If hyperkalemia is significant, changes to the EKG might include:
-
- slow heart rate (the 4 beats below might only be 2-3 beats)
- absent P waves
- widening (prolonged) QRS complex
- Shorter (decreased amplitude) R wave
Our heart page has much more information on EKG’s.
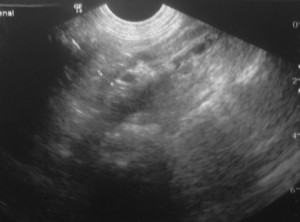
Ultrasonography
Ultrasonography would usually show small adrenal glands, although a dog can have Addison’s and have normal adrenal glands on ultrasound. The adrenal glands in Addison’s are tiny, and can be difficult to find in some cases.
This is a normal right adrenal gland enlarged for easier viewing. It is marked by the + signs.
This is a small left adrenal gland like we might find in Addison’s. It is the whitish area in the center towards the top with the dark area in the center. It takes an experienced ultrasonographer to find a small adrenal gland.
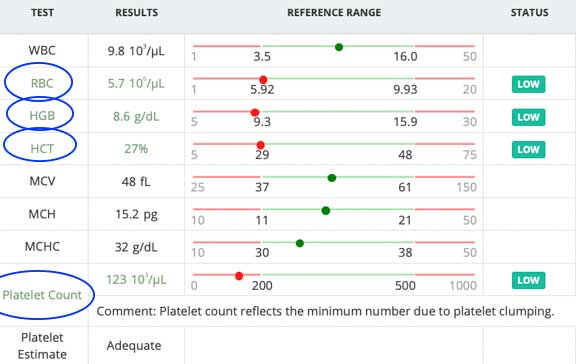
Blood Panel
Blood work (chemistry and complete blood count) is a crucial component for detection of this disease. Common abnormalities might include one or more of these findings:
-
- anemia (low red blood cells)
- increased eosinophils (eosinophilia) and lymphocytes (lymphocytosis)
- lack of a stress leukogram
- low blood sugar (hypoglycemia)
- azotemia (high BUN and creatinine)
- hypercalemia (high calcium)
- hyperkalemia (high potassium)
- hyponatremia (low sodium)
- hypochloremia (low chloride)
- increased liver enzymes (ALT)
- increased alkaline phosphotase (ALP)
- hypoalbuminemia (low albumin)
- hypocholesterolemia (low cholesterol)
- low ratio of sodium (Na) to potassium (K). If the ratio is less than 27:1, and the history and symptoms are consistent with this disease, then a high index of suspicion is appropriate.
Cortisol decreases the blood flow (also called GFR-glomerular filtration rate) to the kidneys. This will result in an decrease in the amount of water and waste products filtered by the kidneys. On the blood panel this might show up as kidney disease, when in reality it is Addison’s. Our kidney disease page has more details.
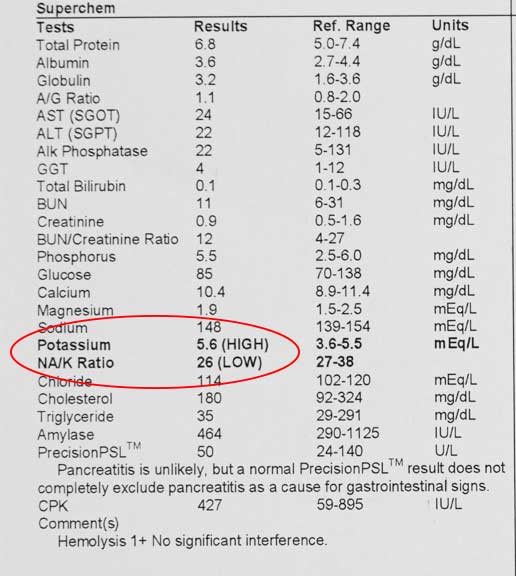
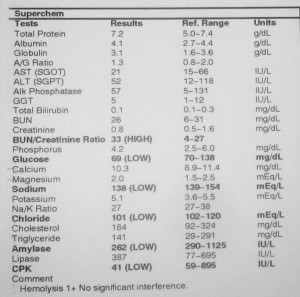
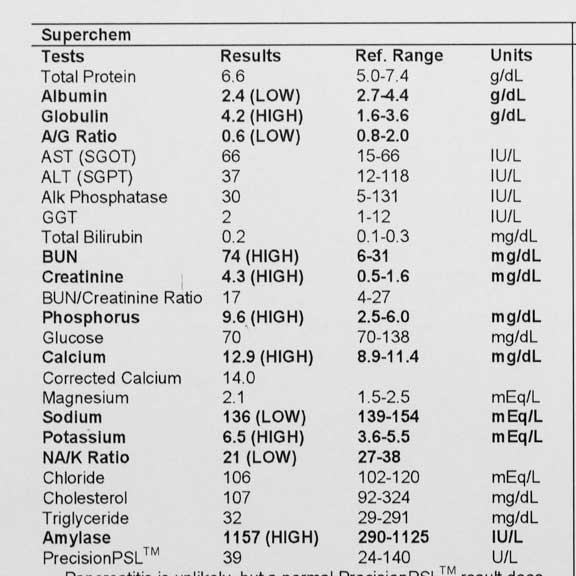
Each of the following blood panels was taken from a dog with or suspected of Addison’s. They are all different, a testimony to how variable this disease can appear on a blood panel. When coupled with the wide variety of symptoms, that can wax and wane, a diagnosis of this disease is not black and white.
The low RBC (Red Blood Cells), HGB (Hemoglobin), and HCT (Hematocrit) are all indications of anemia on this dog CBC blood test, could be a sign of Addison’s
This dog has a low Na/K (Sodium to Potassium ratio) that could indicate Addison’s. Further testing is warranted in this case to confirm.
In this dog that does have Addison’s, the chloride, sodium, and glucose are low. The Na/K ratio is OK.
This sick dog with Addison’s has numerous abnormalities, causing it to be very ill. It needs emergency treatment, including fluids and medication for Addison’s.
We prefer not to wait until your pet is this ill before we diagnose and treat this disease. That is why the earlier blood panel, showing only a low Na+/K+ ratio on a healthy pet, should be performed as part of a yearly Wellness Exam. Catching this problem at this early stage, and before your pet becomes so ill as to have the blood panel with many abnormalities, is our goal.
If by chance you find yourself in an emergency situation with an ill pet, the Long Beach Animal Hospital is staffed with emergency vets, available until the evenings 7 days per week. If you have an emergency always call us first (562-434-9966) before coming in so that our veterinarians can advise you on what to do at home and so that we can prepare for your arrival. Now might be a good time to read our Emergency Services page.
Special Tests
Cortisol level
In this test a baseline cortisol level is run by taking a blood sample. If the baseline cortisol is over 2 mcg/dl (micrograms per deciliter) then the dog does not have Addison’s. There is no need to go any further since Addison’s is not involved at this point. If the baseline cortisol is less than 2 mcg/dl then we will do the ACTH stimulation test.
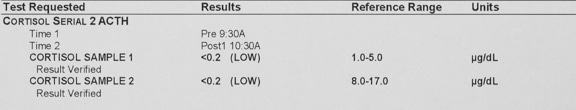
ACTH Stimulation test
Diagnosis is confirmed with an ACTH (adrenocorticotrophic hormone) stimulation test. This test is also used to help diagnosis the opposite problem of Addison’s disease, which is called Cushing’s disease.
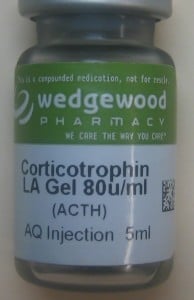
This is a picture of the bottle we use to inject the ACTH
Once the baseline blood cortisol is obtained we give an injection of a specific amount of ACTH. One hour later we take another blood sample to check if the cortisol level has changed. We get the reports from the lab usually the next day.
If the baseline cortisol is less than 2 mcg/dl, and it does not increase on the blood sample taken one hour later after we have injected ACTH, then the disease is confirmed.
This ACTH stimulation test confirms Addison’s in this dog
Akita’s and Shiba inu’s sometimes have elevated potassium levels on blood tests. This can be very confusing when a patient has symptoms that suggest Addison’s disease. The ACTH Stimulation test will let us know if they have Addison’s.
An occasional dog will be presented with symptoms consistent with Addison’s, including abnormal sodium and potassium levels. These dogs might have Whipworms and not Addison’s. Again, the ACTH Stimulation test will let us know if they are Addisonian. We have a page on internal parasites that includes Whipworms.
Treatment
Acute Phase
In the acute phase, dogs are presented collapsed and in a state of shock and hypothermia. They need shock doses of intravenous fluids and injectable cortisone (dexamethasone) along with warmth. If the hyperkalemia is causing bradycardia, the IV fluids usually suffice. If not, insulin needs to be administered to help lower the potassium. If hypoglycemia is present, dextrose is added to the IV fluids.
Chronic Phase- Most dogs are presented in this phase
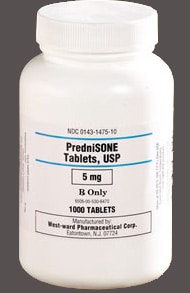
For low cortisol we use prednisone orally at a relatively low but consistent dose. Any pet with chronic Addison’s needs to have this dose increased when there is a stress like fireworks, going to the groomer or veterinarian, or anything in general that causes extra stress.
We like to monitor the electrolytes at 14 and 28 days once we start your pet on prednisone, and adjust the prednisone dose accordingly.
We will test the blood every 6 months at the least to make sure there are no serious side effects to this use of cortisone. We use the lowest does possible, so for the majority of dogs, there are no side effects, and the drug is mandatory for treatment of this disease. The symptoms of the disease, and their potentially life threatening nature, far outweigh side effects when used under our supervision.
Prednisone and prednisolone are tried and true drugs that have been used to treat this disease for many decades
For an imbalance in electrolytes we use one of two drugs, although the injectable version is much more convenient and very effective:
Percorten-V (DOCP- Desoxycorticosterone Pivalate) or Zycortal
This is a mineralocorticoid replacement drug that is a precursor to aldosterone. You learned about how important aldosterone is in regulating electrolytes like sodium and potassium in the physiology section above. It works on the collecting ducts and tubules in the kidneys. It increases serum sodium and chloride, and decreases potassium by enhancing its excretion in the kidneys.
Percorten-V works extremely well for most dogs and allows them to lead a normal quality of life. This injectable medication is given every 25 days for the majority of dogs. We will test the electrolyte levels with a blood panel early in the course of treatment to monitor Na and K levels and adjust the timetable accordingly. We will then test the blood at least every 6 months.
Harmony is drawing up Buddy’s Percorten
Buddy comes in every 25 days on the dot, and after his pinprick injection (we use a 25 gauge needle so it is jut a pinprick) he is good to go for another 25 days.
If we start your pet on this drug we want to monitor its effects in 10-14 days by checking the electrolytes. If the low sodium and high potassium are still present we will increase the does by 10-25%. We will decrease it by the same amount of the sodium is high and the potassium is low.
Florinef – It does have some cortisone properties, and in some cases a dog does not need prednisone when on this drug. This does not apply to stressful situations, and additional medication in the form of prednisone tablets is always needed.This oral medication has fallen out of favor as a treatment because it has to be given daily, and some dogs develop a resistance wherein the dose has to be increased.
The pills are small and easily given
Prognosis
This is a hormone disease, which means it is part of a highly tuned and refined mechanism that is in constant state of change. Vigilant monitoring is of essence for a successful outcome. We have numerous dogs at our hospital currently being treated successfully with prednisone and Percorten-V over many years.
These dogs are leading a normal life, and you would have no idea they have a serious hormone disease when you see their owners bring them into our hospital or take them for a walk.