One of the more common conditions encountered in pets, especially as they age, is kidney (renal) disease. This disease is particularly prevalent in older cats, and is called chronic renal failure (CRF).
Cats that have kidney disease commonly have other problems that need careful attention if the kidney problem is to be treated successfully. Some of these other common problems are hyperthyroidism, heart disease, dental disease, sugar diabetes (diabetes mellitus), and high blood pressure (hypertension) leading to blindness.
Renal anatomy
The kidneys are such a vital organ that 25% of the blood that enters the circulatory system from each heartbeat goes directly to the kidneys through the renal artery. With such a high metabolic rate the proper functioning of this organ is critical to health. The high metabolic rate and importance of this organ makes the kidneys susceptible to many problems.
This is a typical kidney found in mammals. Blood enters the renal artery and flows into the nephron where it is filtered (the rectangular box outlines where a typical nephron is located). The blood from the renal artery that has been filtered now flows out of the renal vein where it goes back into the circulatory system. The impurities that the nephron filters out of the blood collect in the pelvis and eventually out into the ureter in the form of urine.
The primary functional unit of the kidney is the nephron (outlined as the black rectangle in the above picture). Each kidney has upwards of one million, so obviously they are microscopic in size. Every nephron is a self contained unit that can form urine by itself. Not all nephrons are used at the same time, which gives the kidneys the capacity to increase their workload if called upon. This reserve capacity is lost when chronic renal failure occurs. These pets (especially cats) outwardly appear normal, but have greatly reduced ability to adapt to changing physiologic needs. Being chased by a dog, not having enough water to drink, etc., can send them into renal failure.
Renal Physiology
The kidneys have a profound affect on almost all the physiologic processes of the body. The mechanism by which the kidneys perform these functions is extremely complex, the most important of which will be summarized:
Fluid Regulation
In relation to the kidneys, the brain monitors bloodstream levels of water, waste products, electrolytes, and red blood cells. The circulatory system has receptors like the brain to monitor blood volume also. If the water level is too low, as occurs with dehydration, the brain secretes more of a hormone, called ADH (anti-diuretic hormone), into the bloodstream. As a result, the kidneys excrete less water into the urinary tract, retaining more fluid in the bloodstream to counteract the dehydration. The brain also increases thirst simultaneously. The end result is less urination. The urine that does get excreted is more yellow than usual due to a greater concentration of waste products being excreted in relation to the amount of water being excreted. The only thing we notice is that we urinate less and it is more yellow in color.
As we drink water to quench our thirst and rehydrate, the body notes this change and the brain secretes less of the hormone called ADH. Now when we urinate more water is excreted by the kidneys, and our urination occurs with a dilute urine in greater quantity. So, the ability to concentrate the urine and dilute the urine is an important function of the kidneys. It is a fine tuned mechanism that is closely regulated to maintain optimum amounts of fluid in the bloodstream and organs.
As a fun fact, it is the inhibition of ADH by alcohol’s depression effects on the brain that causes excess urination when drinking alcoholic beverages. Eventually this excess urination causes dehydration, leading to that inevitable curse called a hangover.
Waste Product Regulation
The brain also monitors waste products that build up in the bloodstream. These waste products are the end product of normal metabolic processes, especially the metabolism of proteins. They are called nitrogenous waste products, and are measured by a blood parameter called blood urea nitrogen (BUN). Another waste product that is closely regulated by the brain and kidneys is called creatinine. It is the end product of the metabolism of muscle.
The kidneys also excrete toxins and foreign substances that are introduced into the body. Almost every medication given, either orally or by injection, is eliminated to some degree by the kidneys.
The rate at which fluid flows into the glomerulus is important. This is called the glomerular filtration rate (GFR), and is measured in ml/minute. Too small a flow and waste products are not eliminated, a problem encountered during dehydration. Too much flow and normal blood constituents like protein are excreted when they shouldn’t be.
Electrolyte Regulation
Electrolytes are also of importance in relation to the kidneys. Sodium is of extreme importance in the normal functioning of all cells. It allows nerve impulses to occur and is critical in the regulation of water levels in the bloodstream. Through the release of a hormone called angiotensin the kidneys regulate fluids levels of sodium in the bloodstream. This has a major affect on the blood pressure. Potassium is also a critical electrolyte. Potassium levels need to be kept at a very narrow range to prevent serious consequences like heart irregularities.
The kidneys also regulate calcium and phosphorous by a hormones called calcitrol and parathyroid hormone, and by regulating vitamin D. The pH of the bloodstream, which is a measure of acidity, is another important area of kidney physiology.
Red Blood Cell Production
The kidneys secrete a hormone called erythropoeitin into the bloodstream. This hormone circulates to the bone marrow and stimulates it to produce red blood cells. A lack of adequate levels of this hormone will cause anemia. Toxic waste products that build up in the bloodstream decrease the life span of a typical red blood cell, further exacerbating the anemia.
Pathophysiology of Chronic Renal Failure
Over the course of days, weeks, or months, normal nephrons get replaced with scar tissue, and become non-functional. When this occurs to approximately 75% of the nephrons the kidneys no longer have the ability to respond to the needs of the body. There is no longer any reserve, and all of the remaining nephrons are working full time. Eventually these remaining nephrons can not keep up, and it leads to a buildup of nitrogenous waste products (called azotemia) in the bloodstream. The body compensates by increasing thirst, which causes PU/PD, and the waste products get flushed out of the bloodstream and into the urine. Unfortunately, flushing out the waste products in bloodstream with excess thirst also flushes out important electrolytes and protein into the urine. This causes weight loss and weakness as the kidneys continue to deteriorate. The excess urination that occurs as the body tries to rid itself of these excess waste products can also cause dehydration.
Oral ulcers occur when bacteria in the mouth convert the extra uremic waste products to ammonia. Waste products that buildup in the bloodstream also have an effect on the bacteria in the mouth and exacerbate gingival and periodontal disease. The waste products also change the pH of the bloodstream and cause ulcers in the stomach and intestines. This causes vomiting (emesis), loss of appetite (anorexia) and weight loss. Ulcers can also be found in the mouth and tongue due to the uremia.
Hormones are affected and phosphorous builds up in the bloodstream further adding to a pet’s woes. Eventually calcium is deposited in abnormal places, and can lead to problems with many skeletal and internal organ problems. Due to sodium imbalance hypertension (high blood pressure) can develop.
As the kidneys continue to deteriorate erythropoetin is not secreted in adequate quantity and anemia results. This anemia also makes a pet weak and adds to the anorexia that is usually present.
The nervous system is affected by all of these problems. If the uremia is severe enough hypothermia and seizures can result.
Classification
Acute Renal Failure (ARF)
This is a serious form of kidney disease that commonly leads to death. The kidneys have an abrupt decrease in the GFR due to a toxin or loss of adequate blood supply (called ischemia). Many different disease processes can cause ARF.
Chronic Renal Failure (CRF)
This is the most common form of kidney disease we encounter, particularly in older cats. It tends to develop more slowly than ARF, so the body has time to institute corrective factors (called homeostasis) to compensate for the problem. Unfortunately, these corrective factors tend to hide early symptoms of disease. Consequently, treatment is not initiated as soon as it might be. Again, as in many diseases we encounter, this drives home the fact that pets over 8 years of age should have annual physical exams along with blood and urine samples.
Pets in CRF that have lost their ability to compensate for their failing kidneys can be presented to us in an acute phase, similar to ARF.
Cause
The are a multitude of causes to kidney disease:
- Toxins
- Cancer
- Poor Perfusion
- Cysts
- Immune System Diseases
- Parasites
- Viruses
- Bacteria
- Trauma
Symptoms
The symptoms that occur depend mainly on how long the problem has been present and the specific reason the kidney failed in the first place. Some of the more common ones you might notice at home are:
- Excess urinating and drinking
- Weight loss
- Poor appetite (anorexia)
- Weakness
- Vomiting (emesis)
- Seizures
- Ulcers

Blindness can occur due to the high blood pressure (hypertension) that develops as a consequence of CRF. We start therapy in cats when the pressure exceeds 170 mm.
The dilated pupils from this 15 year old cat with CRF are due to blindness.
Checking a cat for high blood pressure is not as simple as in a human. Specialized equipment is needed, including a doppler ultrasound.
Diagnosis
Since the symptoms of kidney disease mimic the symptoms of other diseases a thorough approachis needed to differentiate them. In every disease we encounter we follow the tenet’s of the diagnostic approach to ensure that we make an accurate diagnosis and that we do not overlook some of the diseases that are also encountered in pets that have renal disease. Unfortunately, it is difficult to diagnose acute renal failure early in the course of disease.
Signalment
Kidney disease can occur at any age. If it occurs at a young age we tend to think more of toxins, cysts, and trauma. The most common form of kidney disease, CRF, occurs mostly in older pets.
History
Kidney disease is suspected in any pet that has some of the symptoms described above, especially PU/PD. The recent administration of medication, a recent bout of a disease, the changing of antifreeze, especially in the fall , and recent administration of anesthesia are all helpful clues. Pets that have other diseases that can affect the kidneys, notably heart disease, and hyperthyroidism, alert us to the potential for kidney disease.
Physical Exam
Symptoms noted during a physical exam depend on what caused the kidney’s to fail, how long the disease process has been present and whether a pet has the acute form or chronic form of the disease.
Physical exam findings might include:
- Pale gums due to anemia
- Dehydration
- Small and irregular kidneys upon abdominal palpation if CRF is present
- Large or nodular kidneys if a cyst or cancer is present
- Underweight
- Enlarged lymph nodes
- Dilated or uneven pupils
- Weakness
Diagnostic Tests
Kidney disease can only be diagnosed with appropriate tests. as a general rule, we recommend screening for kidney disease by running a blood panel and urinalysis on all pets greater than 8 years of age. We also screen for other diseases, notably liver disease, sugar diabetes, andhyperthyroidism, on this blood panel due to their prevalence in older pets.
Lymph node biopsy
Peripheral lymph nodes can be palpated in numerous locations. They can enlarge for several reasons, one of the more important ones is cancer. If they are enlarged and significant disease process is suspected then one of them is biopsied (example to follow).
Blood Panel
An important tool in the diagnosis of kidney disease is a blood panel. We look for abnormalities in several specific tests:
-
BUN-Blood Urea Nitrogen
The BUN can also elevate in dehydrated pets and in pets with an obstructed urethra causing an inability to urinate. Liver disease can also influence the level of BUN. The BUN must be interpreted in conjunction with a urine test called specific gravity.
-
Creatinine
It is a very accurate way to diagnose kidney disease, and is more reliable than BUN since factors like dehydration are not as influential on creatinine as they are on BUN.
-
Phosphorous
In the more advanced stages of kidney disease the phosphorous levels elevate.
-
Amylase
This is an enzyme produced by the pancreas to aid in the digestion of carbohydrates. It is excreted by the kidneys, so an excess could indicate kidney disease
-
Red Blood Cells
The kidneys produce a hormone called erythropoeitin that stimulates the bone marrow to produce red blood cells. Anemia occurs in kidney disease due to inadequate levels of erythropoeitin, shortened survival time of red blood cells in general, bleeding in the stomach or intestines, and the effects of uremic toxins on parathyroid hormone. Pets that are dehydrated might not show anemia on a blood sample until they are rehydrated.
This dog has white gums in addition to the severe dental disease that is present. The white gums are due to anemia from CRF.
This is an actual blood panel from a typical pet with severe CRF. The 3 most important tests on this panel are highlighted in yellow, along with their normal values on the right.
Urinalysis
This is also an important tool in the diagnosis of kidney disease. Changes in several parameters could indicate kidney disease:
-
Specific Gravity (S.G.)
The ability of the kidneys to dilute and concentrate the urine is an important parameter to monitor. Water has a specific gravity of 1.000. A pet with kidney failure has a specific gravity of between 1.008-1.012. In cats with normal kidney function, the S.G. should be greater than 1.034, in dogs it should be greater than 1.025.
This number is interpreted in conjunction with the BUN to help determine if the elevation in BUN is due to dehydration or kidney disease. To complicate things further, dehydration and kidney disease can occur simultaneously. Also, as mentioned above, liver disease, a common problem in older pets, can also be an influence.
-
Protein
Excess protein in the urine, called proteinuria, can occur in glomerulonephritis, pyelonephritis and amyloidosis.
-
Cells
Specific types of cells, called casts, can also be an indication of kidney disease.
This urine sample is from the cat with the blood sample shown above. The S.G. is very low, and since this cat has a high BUN, the problem is most likely due to CRF. Fortunately for this cat there are no other serious abnormalities on this urine sample.
Radiography
Radiography can be very helpful in the diagnosis of kidney disease. It allows us to visualize the kidneys, check for stones in the urinary system, look for calcification that might go along with kidney disease, and also look at other organs that commonly have a problem as pets age.
This is the radiograph of a cat with normal kidney’s that is laying on its right side. The right kidney (RK) usually lies forward in the abdomen compared to the left kidney (LK). The area of the 2 kidney’s that overlaps is more whitish in nature.
These kidneys have a normal size and shape. Use this for comparison purposes as you look at the other radiographs.
This is the radiographic of a cat with renal lymphosarcoma (malignant cancer). The diseased kidney is the large white circular area in the center of this view. It is pushing the large intestine down.
Ultrasound
A very valuable tool in the diagnosis of kidney disease is ultrasound. It allows us to look at the internal anatomy of the kidney, measure kidney size, and take a biopsy for an accurate diagnosis. In many cases the use of ultrasound precludes us from having to perform an exploratory surgery.
These ultrasound pictures are from the first cat above with the enlarged kidneys. The first picture shows a normal right kidney. Its measurements are 2.3 cm by 3.6 cm.
The 2nd image shows the large and cancerous kidney, measuring 4.6 cm by 7.3 cm. A biopsy was taken from this kidney to confirm the diagnosis of renal lymphosarcoma.
Excretory Urogram
This special test, also know as an IVP (intravenous pyelogram) gives us significant information about the renal system. It has to be used carefully if ARF or CRF is suspected because it can exacerbate the problem. A radiopaque dye is injected into the bloodstream and radiographs are taken of the dye as it passes through the kidneys, ureters, and bladder.
This picture shows how the dye outlines the center of each kidney, called the renal pelvis (remember the renal pelvis in the anatomy picture at the beginning of this page?).
Laparotomy
Exploratory surgery (laparotomy) is frequently used as an aid in the diagnosis and treatment of renal disease, especially cancer. We use this option when we feel that ultrasound will not be advantageous.
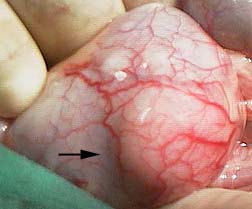
The arrow points to a lump on the surface of a kidney. It was caused by cancer that spread from the stomach.
A section of the lump was biopsied during surgery to determine the cause. The tremendous blood supply to the kidneys can easily be visualized.
Three sutures were placed in the kidney to control the bleeding that occurred at the biopsy site.
A biopsy of a lymph node (called cranial mesenteric) located in the center of the abdomen was also obtained. This helps us determine if the cancer has spread.
Treatment
Acute Renal Failure
This form of renal disease needs immediate and aggressive treatment to prevent death. Any drug suspected of causing the problem is stopped immediately, and underlying problems are addressed.Fluid therapy is critical, and consists of saline and dextrose solutions initially. Fluid therapy corrects fluid and electrolyte imbalances, increases the blood flow to the kidneys, and starts the process of diuresis.
Cats need to maintain their caloric input in order to minimize the metabolism of protein for their caloric needs. Metabolizing excess of amounts of protein will increase uremia, causing a further deterioration in condition.
Pets that are still not urinating after this initial fluid therapy are given Lasix or mannitol. Excess potassium (hyperkalemia) is a common finding in aRF. If mild, fluid therapy alone should correct the problem. If severe, regular insulin and sodium bicarbonate are used. Pets with ARF are sensitive to ulcers and infections, so treatment for these problems is sometimes initiated. Ethylene glycol (antifreeze) poisoning is an example of ARF.
Chronic Renal Failure
This is the version of kidney disease we encounter most often. The prognosis is guarded, and depends significantly on how long the disease process has been present along with your pet’s age. Pets that have other diseases that are common at this age can make this difficult to treat if not caught early enough.
Many pets (especially cats) that are brought to our hospital have CRF that has progressed to the point where the problem has become similar to ARF. These pets need to be hospitalized and put on intravenous fluids almost continuously to get them over this acute phase. We will closely monitor their BUN and creatinine before therapy is instituted and during hospitalization to ascertain if their kidneys are responding to fluid therapy. If the BUN and creatinine do not drop significantly after 24-48 hours of intravenous fluids then the prognosis for recovery is poor.
Many treatments have been advocated to help minimize the symptoms of CRF (also called the uremic syndrome). None of them can cure the problem, and not all of them have proven to work, so it is important that we tailor make each pet’s therapy to its individual needs. In addition, indiscriminate use of medication to treat a perceived problem can make the kidney disease worse. This applies to almost every drug, since the kidneys are so intimatley invovled in the metabolism of drugs. The medical axiom of “first do no harm” applies directy to kidney disease.
Diet
Pets with CRF need to be fed a diet that has limited amount of high quality protein. Less protein in the diet leads to less work the kidneys have to perform by removing the nitrogenous waste products that are the end result of protein metabolism. Protein is vital to all bodily functions and can not be indiscriminately limited. as a matter of fact, if protein restriction is not implemented carefully it can make the uremic syndrome worse.
High quality protein means that it contains more essential amino acids, which are those the body can not produce and must be obtained in the diet. The commercial food that we recommend for kidney disease is called K/D©. It is made by Hills© and is available only from a veterinarian because it is used to treat a specific disease. In addition to high quality protein it also has less phosphorous.
Most cats take readily to K/D, although it can sometimes be difficult to change the diet on an older cat. Many of the cats are eating poorly and have already lost weight due to the kidney disease, so we don’t want to add to their problem by feeding a diet they won’t eat. Mixing this new food in partially with the regular diet and heating it up a little (for the canned food) in the microwave helps. adding a small amount of a tasty fluid like clam juice can make it taste better.
Water soluble vitamins (ex.- B-complex vitamins) are easily depleted in a pet that has PU/PD. Supplementation can be helpful.
Do not use foods that are lableled “for urinary health”. They are treating a different problem called FLUTD. These foods change the pH of the bloodstream in a way that is detrimental to the kidneys.
Phosphorous lowering medication
Pets with CRF might have an increase in their phosphorous levels as the disease progresses. This excess phosphorous can add to the anemia is common with CRF. It will also dramatically influence calcium metabolism in the body through a hormone called parathyroid hormone. The end result will be painful calcium deposits in the bones and internal organs, including the kidneys.
Antacid type medications will bind to the phosphorous and keep the level in the bloodstream down. We use amphogel© because it is readily available over the counter, it is a liquid, and cats tolerate it well. as already mentioned, K/D© is restricted in phosphorous, and should be used in combination with phosphorous binding medication.
Potassium increasing medication
Pets with CRF will have a decrease in their potassium levels as the disease progresses. This does not always show up on a blood panel. Using oral supplements and adding additional potassium to fluids helps counteract this problem. Oral potassium is called Tumil-K©, and it comes in a paste for easier administration.
Anemia fighting medication
One of the long term affects of CRF is anemia due to a lack of erythropoeitin from the kidneys. This hormone can be supplemented to help minimize anemia. Unfortunately, the body might eventually makes antibodies to this oral medication and the anemia returns, sometime in a more severe form. Use of this medication requires adhering to specific protocols and close monitoring.
Fluids
One of the most important treatments for CRF is the administration of fluids. If your pet is hospitalized we will give them intravenously (IV) because of greater effectiveness and accuracy. If your pet responds to IV fluids during its hospitalization we will initiate the use of subcutaneous (SQ.) fluids at home on a daily basis.
This area of home treatment is so important that we have devoted a complete page to its use. Please click here to learn about the proper technique, then return to this section for more treatment options.
Most cats with CRF should receive between 50 ml and 100 ml of SQ fluids at least several times per week. As the problem progresses it will become necessary to give this fluid on a daily basis.
Blood pressure medications
Hypertension is a common occurrence as the disease progresses. Blood pressure lowering medications like Norvasc and Enalapril will help counteract this problem. All cats initially diagnosed with CRF should have a blood pressure taken. It should be rechecked at least every 6 months.
Anti-ulcer medication
Some cats with CRF don’t eat well because of nausea due to excess hormone secretion in the stomach. Tagamet or famotidine is used to counteract this problem. If we suspect an ulcer in the stomach due to the toxins that have built up we will use Tagamet also.
Anti-vomiting medication
Vomiting is a common problem in pets with CRF. It occurs as a result of uremic toxin buildup in the bloodstream and alterations in hormones that regulate gastric secretions. We use a drug called Reglan to alleviate vomiting symptoms.
Miscellaneous treatments
There are other supplements and medications used in CRF that might be of some benefit, although this is unproven. As long as they do not cause the problem to worsen they might be worth trying.
Appetite stimulants
They are used in older pets in general so their use in CRF might be helpful.
Anabolic steroids
They are also used in older pets for arthritis and appetite stimulation with good success. They might help counteract the affects of anemia, although this can not be relied upon.
Kidney Transplantation
At some select veterinary universities a new kidney can be transplanted into a cat. This does not cure the problem, it is a help in controlling the problem in cats that are losing weight and are anemic in spite of medical therapy.
This specialized surgery can cost upwards of $5,000. Your cat has to be kept on immunosuppressive therapy (cyclosporine and prednisone) the rest of its life, and the donor cat has to be adopted. Complications can occur, especially rejection of the new kidney.
Fresh water should be available at all times. You should fill the water bowl at least 3 times per day to help stimulate drinking. Undue stress should also be minimized at all times.
Prognosis
Pets presented with renal disease, whether ARF or CRF, carry a guarded prognosis. It can be successfully controlled in most circumstances, especially if the diagnosis is made early enough. If your pet is hospitalized with CRF we will closely monitor its blood panel, paying special attention to BUN, creatinine, and phosphorous. If the excess levels of these tests decrease dramatically during hospitalization, and your pet improves clinically, then the use of medications and SQ. fluids at home are usually advantageous.
All pets that have been diagnosed with CRF should have a blood panel, a urinalysis, and physical exam performed every 3-6 months. This disease will progress, and other diseases might present themselves, so this type of monitoring is crucial for a good quality of life.