This page summarizes the complex disease know as Cushing’s disease, also know as hyperadrencorticism. It is a disease that occurs from the overproduction of cortisone by the adrenal glands.
It is the most common endocrinopathy (hormone disease) encountered in older canines. This disease is the exact opposite of another endocrine problem in canines called Addison’s disease (hypoadrenocorticism).
After you read this page you might want to read our much more detailed page on Cushing’s Disease.
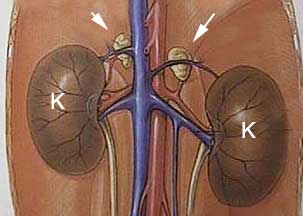
Anatomy
The adrenal glands are small paired glands buried in fat in the front of each kidney. Even though these glands are small, the cortisol they secrete, along with their other functions, have great significance to normal physiology.
The arrows point to the paired adrenal glands in front of each kidney. The extensive blood supply to the kidneys and adrenal glands is apparent. In the diagram they are easy to see. They are not so easy to see during ultrasound or exploratory surgery because normally they are small and buried in fat. They do not show up on an X-ray unless they are calcified.
This is a normal ferret left adrenal gland (just above the hemostat) buried in fat. The left kidney is the structure to the right.
The internal architecture of the adrenal gland is made up of several distinct zones.
-
Cortex
This is the section that produces the glucocorticoid cortisol. Cortisol has large effects on carbohydrate and protein metabolism.
-
Medulla
This consists of the very center of the adrenal gland. It secretes hormones commonly known as epinephrine or adrenaline.
Physiology
These tiny organs have a profound influence on many internal organs. The hormones they secrete work in unison with other internal organs, particularly the liver, and have a profound effect on the body. They also interact with many other hormones that have the opposite effect, usually in some type of feedback mechanism that is monitored by the brain. This interaction is complex, so a summary of adrenal hormone physiology is presented.
The adrenal glands secrete several important hormones, most of which originate from cholesterol. The most important hormone secreted in relation to Cushing’s is called cortisol.
Cortisol, also commonly known by the slang term “steroids”, is a hormone that is essential for life. Cortisol maintains a normal blood glucose level, facilitates metabolism of fat, and supports the vascular and nervous systems. It affects the skeletal muscles, the red blood cell production system, the immune system, and the kidney system.
Stress will increase the level of this hormone in the bloodstream. This includes surgery, infection, fever, and hypoglycemia (low blood sugar). The level of this hormone continually fluctuates in the bloodstream depending on physiologic needs. This continual fluctuation adds to the difficulty of diagnosing Cushing’s, which you will learn about soon.
To control the level of these hormones, the hypothalamus and pituitary gland in the brain secrete chemicals into the bloodstream. One of these chemicals is called adrenocorticotrophic hormone (ACTH). It is the amount of ACTH circulating in the blood stream that tells the adrenal glands how much cortisol to secrete.
There is a negative feedback loop that allows the hypothalamus and pituitary gland to refine precisely how much cortisol circulates in the bloodstream. The more cortisol secreted by the adrenal glands, the ACTH secreted. This allows the body to precisely refine the levels of cortisol, and change cortisol levels rapidly due to changing physiologic needs.
Cause of Adrenal Gland Disease
There are three main causes to adrenal gland disease:
- Pituitary Dependent (PD)
- Non-Pituitary Dependent (AT- Adrenal Tumor)
- Iatrogenic
Pituitary Dependent (PD)
Up to 90% of all Cushing’s cases in dogs fall into this category. The pituitary gland is invaded with a slow growing cancer called an adenoma. This causes it to secrete an excess amount of ACTH. The adrenal glands respond to this excess ACTH by enlarging and secreting excess cortisol. It is this excess of cortisol that is circulating in the bloodstream that causes the symptoms we see in this disease.
Non-Pituitary Dependent (AT)
In up to 15% of Cushing’s there is an actual tumor of one of the adrenal glands (sometimes both are involved). It enlarges and secretes excess cortisol in the bloodstream.
The benign version of this tumor occurs 50% of the time, and is called an adenoma. The malignant version, which occurs the other 50% or the time, is called an adenocarcinoma. It can spread from the adrenal gland to the liver, lung, kidney, and lymph nodes.
Iatrogenic
Long term use of supplemental cortisone, in oral, injectable, or even topical form, might cause an animal to have the symptoms of Cushing’s disease. A common supplemental cortisone is called prednisone. The blood level of cortisone that results from this supplemental use will cause the adrenal glands to shrink in size.
This is because the negative feedback loop tells the brain there is plenty of cortisol in the bloodstream, so the pituitary secretes less ACTH. The pet has the symptoms of Cushing’s because it is being introduced into its body, not because the adrenal glands are overproducing it.
Symptoms
Some dogs with Cushing’s disease show the classic symptoms, while other show only a few vague symptoms. The classic symptoms are:
Polyphagia- excess appetite.
Polyuria/polydypsia (PU/PD)- This is excess urinating and excess drinking of water. Several other important diseases cause these symptoms also, notably liver disease,kidney disease pyometra, and diabetes mellitus (sugar diabetes).
Pot bellied abdomen.
Thin skin and usually symmetrical hair loss along the trunk. The hair might grow in lighter in color or even be hyperpigmented. Secondary skin infections are common.
Other symptoms could include lethargy, muscle wasting, poor appetite, weakness, and behavioral changes.
Diagnosis
Cushing’s disease has a large effect on the skin. Many skin conditions have similar symptoms, so numerous diseases have to be kept in mind when making a diagnosis. These include hypothyroidism,skin allergies, sarcoptic mange, demodectic mange, and Ringworm.
A thorough approach is needed for a correct diagnosis of Cushing’s. In every disease we encounter we follow the tenet’s of the diagnostic approach to ensure that we make an accurate diagnosis and so that we do not overlook some of the diseases that are also encountered in pets as they age.
Signalment
Cushing’s tends to be a problem that affects older dogs, usually greater than 10 years of age. The disease tends to have a slow and gradual onset, so the early symptoms are easily missed.
Several canine breeds are prone to getting Cushing’s:
- Yorkshire Terrier
- Poodle
- Beagle
- Boston Terrier
- Boxer
- Dachshund
Females and males get it at about the same frequency, neutered pets might be at higher risk of Cushing’s.
History
Cushing’s disease is suspected in any pet that has some of the symptoms described above, particularly the skin symptoms and the PU/PD. It is important to remember that some dogs do not show any symptoms early in the course of the disease. This is another reason for yearly exams and blood and urine samples in dogs and cats 8 years of age or more.
Other findings include skin infections that recur after antibiotic therapy is stopped. Some dogs might be itchy if a skin infection is present.
Physical Exam
Routine physical exam findings might include:
Pot bellied abdomen
The abdomen of this dachshund is pot bellied due to Cushing’s. It could also have been due to fluid buildup from cancer or heart disease. An enlarged liver from a disease other than Cushing’s can cause this also.
An enlarged liver (hepatomegaly) might be palpated, along with smaller muscle mass (atrophy) in general.
Bruising (hematoma) might be observed under the skin, or when a blood sample is obtained.
Skin infections and wounds that do not heal or recur after antibiotics are stopped.
This dog has hair loss with a secondary skin infection called pyoderma
Blood pressure might be elevated. This might cause a detached retina, picked up by an ophthalmic exam.
Heart disease, initially noted with the stethoscope as an increased heart rate, an irregular heart rate, or a murmur.
Diagnostic Tests
Several tests are used as an aid in making this diagnosis. Each test has its advantages and disadvantages.
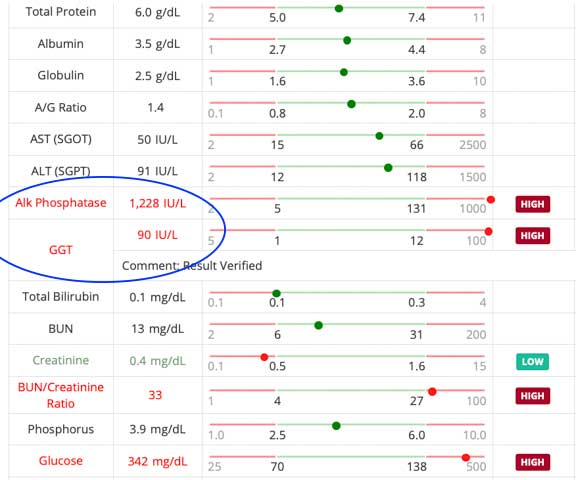
Blood Panel
A CBC (complete blood cell) and biochemistry panel should be run on every dog 8 years of age or more, especially if they have any of the symptoms of Cushing’s.The CBC might show an increased WBC (white blood cell count). The biochemistry panel might show an elevated alkaline phosphatase (Alk Phos).
This is an enzyme that is located in the bile production area of the liver. The excess cortisol influences this enzyme, although other diseases can cause this elevation also.Cholesterol, red blood cells, blood glucose, and liver enzyme tests might also be elevated. If a thyroid test is run also, it might be low or borderline normal.
This dog has a high Alk Phos. Some dogs go much higher than this, especially if the disease has been present for a long period of time. This dog needs further diagnostic tests if there are any other Cushing’s symptoms present also. Note the 3 arrows on the bottom that point to Cholesterol, Bun, and Creatinine. BUN is usually low, not high, in Cushing’s Disease, so this pet might also be dehydrated or have kidney disease at the same time.
This dog has a mildly elevated liver enzyme test and an elevated Alk Phos. If the signalment, history, and physical exam do not make us suspect Cushing’s we probably will not proceed to adrenal screening tests. This dog should be examined, and the blood should be checked every 3-6 months to see if these abnormalities are increasing.
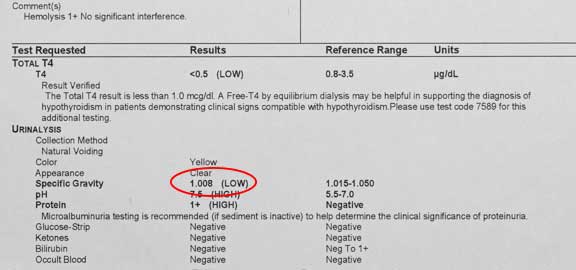
Urinalysis
This test is not as important in Cushing’s disease as it is in other diseases, especially kidney disease. The specific gravity of the urine might be low, the protein might be elevated, and a urinary tract infection might be present because of excess glucose in the urine.
This urinalysis of this Cushing’s dog shows a low specific gravity and excess protein, but the glucose in normal and there is no sign of an infection.
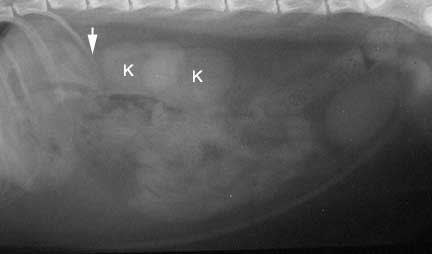
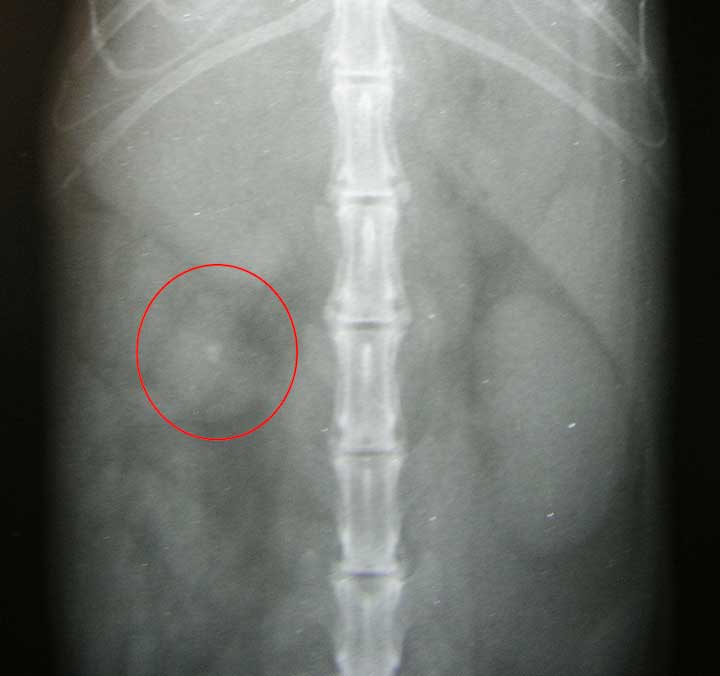
Radiography
Radiography might be of value if the adrenal glands are calcified (might occur with an adrenal tumor), otherwise the adrenals do not show up on a radiograph. an enlarged liver can be seen on the radiograph, along with problems associated with other diseases in pets this age, so a radiograph can be highly beneficial to help rule them out.
In this lateral view (laying on its side) of the abdomen, the kidney (K) closest to the arrow is the right kidney. The arrow points to where the right adrenal gland is located, although it can not be seen since it is not calcified.
In this lateral view (laying on its side) of the abdomen, the kidney (K) closest to the arrow is the right kidney. The arrow points to where the right adrenal gland is located, although it cannot be seen since it is not calcified. The whitish area between the K’s is normal, and is caused by the effect of the 2 kidneys as they overlap.
This is what a calcified adrenal gland might look like on a radiograph
The liver is large and rounded, consistent with a liver problem second to many diseases, including Cushing’s
Ultrasound
This test can be highly beneficial in this diagnosis. The adrenal glands can be measured, and their internal architecture can be analyzed.
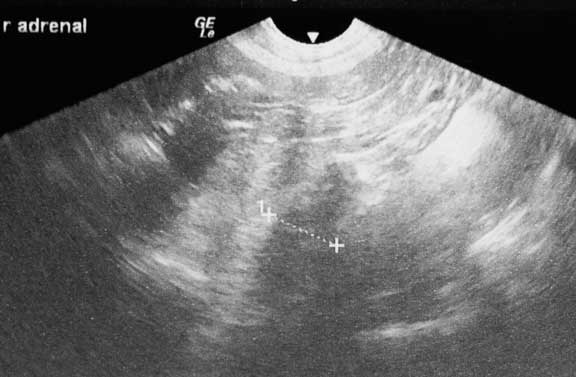
This is the report showing enlargement of both adrenal glands
Screening Tests Background
This is the most reliable way to confirm a diagnosis of Cushing’s disease. These tests evaluate the interactions that are occurring between the hypothalamus, the pituitary gland, and the adrenal gland. The interaction between these glands is know as the hypothalmic-pituitary-adrenal axis.
The first goal is to determine if Cushing’s Disease exists. after this is achieved, the next step is to determine if it is pituitary dependent (PD) or an adrenal tumor (AT).
Testing this axis is not as easy as it sounds. The mammalian body is a dynamic system with thousands of chemical reactions and interactions occurring simultaneously. Also, levels of cortisol are in a continual state of flux, depending on the time of day, the season, medications, diet, and stress levels.
Underlying diseases like Urinary Tract Infections can affect these screening tests, and need to be controlled first. Because of all this variability, interpreting these tests can be problematic, and it is not uncommon to repeat them in the future to look for consistent findings and monitor trends.
Sensitivity
The sensitivity of a test refers to the ability of that test to detect diseased patients. A Cushing’s test that is 95% sensitive will diagnose Cushing’s in 95% of all dogs with Cushing’s disease. 5% of the dogs in this scenario will have Cushing’s, even though the screening test for Cushing’s says they don’t have the disease.
Specificity
The specificity of a test refers to the ability of the test to detect only diseased patients. A Cushing’s test that is 95% specific means that 95% of the time if the test is positive for Cushing’s, the animal really does have Cushing’s. This means that 5% of the time the test will say an animal has Cushing’s disease when in reality it does not.
Animals that do not have Cushing’s disease might show up positive on these tests, while others that have the disease might be negative on these tests. Many times we have to play the odds based on probabilities. Due to this limitation in testing we recommend using these tests in combination, and repeating them if they do not give clear cut answers.
These tests sometimes come back as positive for Cushing’s when in reality other diseases are affecting the cortisol level. Some of these diseases (called non adrenal illness) include liver disease, chronic kidney disease, urinary tract infection, skin diseases, and uncontrolled diabetes mellitus. Also, cortisone and anticonvulsants can give false positives.
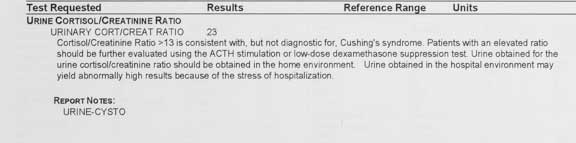
Urine cortisol:creatine ratio test
In this test the level of cortisol in the urine is measured and used as an indication of the cortisol level in the bloodstream. Creatinine is measured to adjust for different levels of urine dilution. Our kidney page has more information on creatinine.
This test is useful as a screening tool when our differential diagnosis (you know what that means because you read theDiagnostic Process page) does not put Cushing’s on the top of the list. For example, we might use it in a pet that has PU/PD, but not the other signs of Cushing’s. It works in both dogs and cats.
This one came back positive, which means this dog might have Cushing’s, and it warrants further testing to confirm. If it was negative, we would probably not do any further testing for Cushing’s, unless we felt the test was improperly obtained, or the dog had significant symptoms of Cushing’s.
This test is easy to perform because all that is needed is a urine sample. We recommend you obtain this sample at home in the morning just after your pet wakes up. Bring it to us immediately for analysis by our lab. Obtaining it at home will minimize the stress of a car ride and a visit to our hospital, both of which will normally increase the level of cortisol in the bloodstream (remember the stress response?), thus affecting this test.
A high level of cortisol in the sample is suggestive of Cushing’s. If the test comes back normal, then it is unlikely that Cushing’s is present.
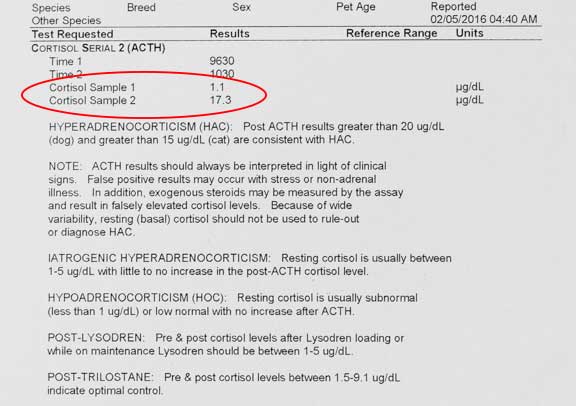
ACTH Stimulation Test
This test checks for Cushing’s and Addison’s Disease. We tend to use this screening test when we suspect Iatrogenic Cushing’s. It is also used to monitor therapy on pet that is on medication for Cushing’s and Addison’s disease.
When a dog or cat is given ACTH by an injection the adrenal glands are stimulated to produce cortisol. By measuring this cortisol with a blood sample we can determine what reserve the adrenal glands have in the production of cortisol.
This is what we use for the ACTH stimulation test
This test is very specific for Cushing’s, so false positives are rare compared to other screening tests. It is not as sensitive as other screening tests, particularly the LDDS test. 20% of dogs that have Cushing’s will be negative on this test. For this reason it is sometimes used in combination with the LDDS test.
This dog does not have Cushing’s according to this test, but it might also be a false negative if the symptoms of Cushing’s are present
A positive on this test gives a reasonably good chance that a dog has Cushing’s. It will not catch all dogs with Cushing’s, so a dog with a negative test might still have the disease.
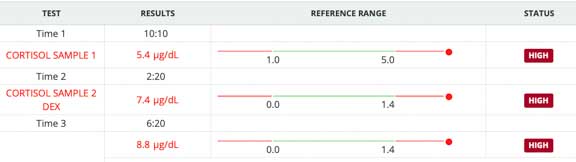
Low Dose Dexamethasone Suppression Test (LDDS)
This is probably the best test when the history, physical exam, and routine blood panel and urinalysis are consistent with Cushing’s. We also use it when we feel there is no chance of Iatrogenic Cushing’s. It might also help differentiate between PDH and AT, but that is better determined by the HDDS test (High Dose Dexamethasone Suppression test). It only works in dogs because cats get a significant number of false positives.
It is sensitive for Cushing’s, because 85% to 100% of the time it finds a Cushing’s disease that is present. This means it does not diagnose a pet that has Cushing’s disease up to 15% of the time.
Its specificity is low though, meaning it might come back as positive for Cushing’s between 44% and 73% of the time when the dog does not have Cushing’s. If we are not sure of the results because of this variability, we might also perform an ACTH stimulate test.
This dose of dexamethasone (which is a version of cortisone) suppresses the adrenal gland from producing cortisol in normal dogs, but not those with Cushing’s. It achieves this suppression by interfering with the negative feedback mechanism. The dexamethasone is monitored by the brain as an excess of cortisone in the bloodstream, so less ACTH is secreted, and therefore less cortisol is secreted by the adrenal gland.
In this test an injection of Dexamethasone is given and cortisol levels are measured at 4 hours and 8 hours after the injection. Like the ACTH stimulation test, a pre-injection blood sample is taken to measure the resting cortisol level.
Here are the LDDS test results on a dog that we suspected of having Cushing’s
Summary of Cushing’s Screening Tests
Urine cortisol:creatinine
In some dogs with Cushing’s the excess cortisol that circulates in the blood stream will spill over into the urine. If this test is positive then a dog might have Cushing’s. If it is negative, there is a good chance it does not have Cushing’s.
ACTH Stimulation
A positive on this test gives a reasonably good chance that a dog has Cushing’s. It will not catch all dogs with Cushing’s, so a dog with a negative test might still have the disease. In general, we use this test to monitor patients that are already being treated for Cushing’s or Addison’s.
LDDS
This test will catch most dogs that have the disease, and is the test of choice for Cushing’s on dogs that have symptoms. A negative on this test means that most likely the dog does not have Cushing’s. A positive on this test indicates that a dog might have Cushing’s. It is the most popular adrenal screening test.
If a dog has symptoms that are typical of Cushing’s, but all of these tests come back negative, we recommend repeating these tests every 1-3 months to monitor.
Treatment For Cushing’s Disease Overview
Before we discuss treatment we need to keep things in perspective. This is a chronic disease, and most dogs do not die from this disease. We tend to treat when the symptoms described previously are affecting a dog’s quality of life or are a major nuisance to a pet owner. We do not routinely treat just because the tests say your dog has Cushing’s- the symptoms of the disease need to be present also.
It might be years before this dog shows signs, if any, of Cushing’s. At the same time, we want to start treatment at the optimal time just as the symptoms of Cushing’s starts. Any dog diagnosed with Cushing’s should have follow up tests performed periodically to look for changes to help in this decision.
Dogs that have significant symptoms of Cushing’s that have been confirmed by screening tests need to be treated to prevent potentially serious diseases secondary to Cushing’s that include Diabetes Mellitus, Urinary Tract Infection (UTI), pancreatitis and High Blood Pressure (Hypertension).
This Staph bacteria was cultured from a urine and numerous antibiotics were tested to find the most effective one. The S means this Staph infection is sensitive to everyone of these antibiotics in this in vitro test. This is a rare occurrence, and shows no antibiotic resistance.
Treatment can be drawn out, and involves significant time and expense to monitor your pet after we treat it. Also, in some dogs, treatment can sometimes lead to side effects that are more serious than the symptoms of this disease. One of these side effects includes a rare death, so we do not undertake treatment of this disease lightly.
Pituitary Dependent (PD) Cushing’s Treatments:
Trilostane
This is the newest treatment for this disease, and the one we recommend in most cases. Trilostane is an inhibitor of an enzyme called 3-beta-hydroxysteroid dehydrogenase. This enzyme is involved in the production of several steroids including cortisol. Inhibiting this enzyme inhibits the production of cortisol.
It will be given daily for the rest of your dog’s life
It is usually given once per day, but in some dogs, especially those with Diabetes Mellitus, the Cushing’s symptoms might not diminish at the once daily dosing and the medication needs to be given twice per day (every 12 hours). It always needs to be given with food for proper absorption. Some dogs do not absorb this drug even when treated with food. In that case, another drug needs to be used.
When we use this drug to treat your dog’s Cushing’s we will also give you a detailed flow chart of what to look for at home and when to return for additional test and monitoring. The ACTH stimulation test is used for monitoring purposes. Do not fast your dog on the day we do this test, and give the Trilostane as you always do.
This flow chart is helpful to monitor the adequacy of adrenal suppression by Trilostane
If your dog does not respond to Trilostane, and the ACTH stimulation test indicates inadequate adrenal suppression, the dose or frequency of administration might need to be changed.
If you are using the compounded version of trilostane, and your dog is not responding, switch to the name brand of trilostane (Vetoryl from Dechra).
Mitotane (o,p’-DDD)
This drug has been used to treat this disease for 30 years, and is know by the trade name of Lysodren. It selectively destroys the zona fasciculata and reticularis, effectively limiting the amount of cortisol that these areas of the adrenal gland can secrete.
Pets that are on insulin for diabetes mellitus need to have their mitotane and insulin doses adjusted downwards. It should be administered with meals to enhance its absorption. This drug is first administered at a loading dose for 7-10 days.
Side effects are not uncommon:
- lethargy
- emesis (vomiting)
- diarrhea
- anorexia (poor appetite)
- weakness
- ataxia (in coordination)
Side effects are due to the cortisol level being reduced below normal levels. Even if the cortisol level does not go below normal levels, a rapid decrease in elevated cortisol levels to the normal range can still cause these symptoms.
You need to closely observe your pet when it is on mitotane for any of the above side effects. If they occur you are to immediately stop medicating and call us. We will already have given you prednisone pills to give at home if side effects are significant.
After 7-10 days of loading dose the cortisol levels are assessed with the ACTH stimulation test. Do not give your pet any supplemental cortisone on the day of testing. The pre and post cortisol levels should be normal. If they are, then we will continue to use mitotane at a weekly maintenance dose to prevent the problem from recurring again. Once your pet gets to this point it is rare to need any supplemental cortisone pills.
Two long term effects can occur while on mitotane maintenance therapy:
- The Mitotane can be so effective that the adrenal glands do not produce enough cortisol for normal physiology. This is called iatrogenic hypoadrenocorticism. In these dogs we stop all mitotane therapy and use supplemental prednisone. Sometimes this side effect is permanent, and your dog needs to be on supplemental prednisone the rest of its life.
- It is not uncommon for relapses of Cushing’s to occur within 12 months, even while on the maintenance therapy. These dogs are again given a loading dose of mitotane, then converted to maintenance dose when cortisol levels are normal.Both of these effects emphasize the need for continual monitoring of your pet. This means close observation at home and ACTH stimulation tests every 3-6 months.
This drug controls the symptoms of Cushing’s 80% of the time.
Feline Cushing’s
Cushing’s in cats is rare compared to dogs. One reason is because they tend to be more resistant to higher levels of cortisol, especially if iatrogenic. Most feline Cushing’s occurs in females. It can affect the ability to control the blood sugar level in cats with diabetes mellitus concurrently.
History
Cats do not show as much PU/PD as dogs do, unless they have diabetes mellitus also. Most cats are presented in a more advanced state of Cushing’s disease because the early symptom of PU/PD is not observed. They might also have hepatomegaly, weight gain, pot-bellied appearance, and muscle wasting. Sometimes the skin is easily bruised and torn. This is called the fragile skin syndrome.
This picture is from an older cat that was at the groomer to be clipped. The skin literally peeled off like wet tissue paper when the groomer attempted to clip some mats. This is a serious problem and does not lend itself to an easy treatment.
Diagnosis
Cats do not routinely show any changes on a regular blood panel or urinalysis. The most consistent finding on a blood panel is hyperglycemia (elevated blood sugar). An elevated alkaline phosphatase occurs in only a minority of cases. Oftentimes the elevated alkaline phosphatase is due to liver changes from unregulated diabetes mellitus.
The urine cortisol:creatine ratio test is helpful in cats, especially since it is a relatively stress free test compared to blood sampling. If the test is normal then there is much less of a chance that Cushing’s is present. It the test is elevated it might be Cushing’s, but there are also other situations that cause this elevation.
The ACTH stimulation test is used, but two blood samples need to be analyzed at 30 and 60 minutes, instead of the 1 sample at 2 hours for the dog. This is because the increase in cortisol is variable in the cat. False negatives are common. False positives occur in stressed cats or those with non adrenal illness.
The LDDS test is used but the dexamethasone that is injected needs to be given at a higher dose. This test, when used in conjunction with the ACTH stimulation test, is one of the best ways to diagnose Cushing’s in the cat.
The HDDS test to differentiate PD from AT has not been refined to the point that is of diagnostic value.
In general, results of these tests can be variable, and must be interpreted in conjunction with the history and clinical findings. In light of the fact that Cushing’s is uncommon in cats, these tests need careful interpretation.
If the above tests suggest Cushing’s then radiology can be helpful since up to 30% of feline adrenal tumors are mineralized. Other radiographic findings include hepatomegaly and obesity.
Ultrasonic evidence of an enlarged adrenal gland (especially if unilateral) or changes in internal adrenal architecture is strong evidence of an adrenal tumor (AT).
Adrenal tumors occur in about 20% of feline Cushing’s. They can be malignant or benign.
Treatment
Medical therapy is generally unrewarding. Ketaconazole can be used, but the effects are variable, and side effects can occur. Mitotane might help, along with metyrapone. Metyrapone may be more helpful as a pre-surgical stabilization prior to surgery. Anipryl has not been used in cats.
Surgery is needed to remove one of the adrenal glands if the gland has a tumor, and both glands if the problem is PD. If both glands are removed the cat has to be on supplemental cortisone (prednisolone) and mineralocorticoids for the rest of its life. Some cats with concurrent diabetes mellitus will no longer have the disease when their adrenal tumor is removed.
Unfortunately, cats with Cushing’s can be poor anesthetic risks due to diabetes mellitus and fragile skin. When this occurs we sometimes will use medical therapy to help control the problem and make our patient a better anesthetic risk.
Emergency Care for Cushing’s at Long Beach Animal Hospital (LBAH)
Even thought it is not often that a dog or cat is presented to us with an emergency due to this disease, if your pet has other medical problems at the same time this is possible. The Long Beach Animal Hospital, staffed with emergency vets, is available until the evenings 7 days per week to help if your pet is having any problems, especially shock, pain, breathing hard, or bleeding.
Think of us as your Long Beach Animal Emergency Center to help when you need us for everything from minor problems to major a major emergency. We serve all of Los Angeles and Orange county with our Animal Emergency Center Long Beach, and are easily accessible to most everyone in southern California via Pacific Coast Hwy or the 405 freeway.
If you have an emergency that can be taken care of by us at the Animal Emergency Hospital Long Beach always call us first (562-434-9966) before coming. This way our veterinarians can advise you on what to do at home and so that our staff and doctor can prepare for your arrival. To learn more please read our Emergency Services page.